Business
MultiPlan, the secret back-end to most of the insurer industry, is going public
Published
3 years agoon
By
admin
In a recent announcement, MultiPlan, an entity offering a shadow provider network to insurers, declared that it was going public through a SPAC. Upon closer inspection, MultiPlan represents some of the worst aspects of American health care.
The world of health insurance is deliberately murky. There are monthly premiums, basically a subscription to access the insurance; deductibles, which are minimum amounts a patient pays before the insurance kicks in, usually in an emergency or surgery setting; and co-pays, which are additional fees the patient pays for the privilege of seeing a doctor, usually $20-70.
All of the patient-side fees are confusing, but the provider-side is even more so. Insurers handle negotiations with doctors and hospitals (and, importantly, negotiating with a doctor does not necessarily mean the insurer has negotiated with the hospital and vice versa) to reach a set price for a specific service. These prices are negotiated down from the hospital or physician’s chargemaster (a list of prices). The chargemaster bears no relation to actual charges but is instead the provider’s best attempt to set a high bar at the outset of a negotiation process. When an uninsured patient is billed an extraordinary amount, it’s usually because they didn’t have the negotiation layer of an insurer built in.
The purported value add of insurers, then, is that they lessen costs for patients by handling catastrophic expenses and negotiating down high provider fees.
For a few reasons, this isn’t wholly true. For one, health systems are increasingly merging with insurers, meaning any “negotiation” on behalf of the patient is happening within two divisions of the same company.
But also, many insurers are doing much less negotiation than they make it seem.
The corporation also uses a Palantir-like combination of algorithm and human to root out “fraud and abuse” in payments.
Three weeks ago, a new merger announcement threw the health care world into a bit of a tizzy. MultiPlan, a complementary PPO network, announced it was going public via a SPAC. The announcement forced quite a few people to start looking up what MultiPlan actually does, including me.
MultiPlan, it turns out, is a corporation that handles a lot of insurers’ work for them. It handles negotiation with providers nationwide and consequently has the largest preferred provider network in the country. This means that insurers can contract with MultiPlan and simply get access to MultiPlan’s network, rather than doing thousands of negotiations. This service is so valuable that all 10 of the top 10 insurers use it, and the corporation seems to have carved out a little monopoly at the top.
MultiPlan didn’t start with so much power. It was founded in 1980 to solve an growing problem: when people traveled, their narrow network insurance plans didn’t follow them. If a person from Delaware had an accident in Colorado, they likely fell out of network and did not receive insurance coverage. To fill this gap, MultiPlan formed a network of “shadow contracts,” negotiated rates with providers that fell outside most networks, and sold this network to other insurance plans.
Over time, as the main insurers became bigger and more national, these shadow contracts became less important. But MultiPlan remained at the top of the insurer network, mostly because the Affordable Care Act of 2010 triggered an avalanche of startup insurers (Oscar, Clover, etc.) while also mandating that insurers cover out-of-network emergency care (although it did not ban surprise billing). MultiPlan offered these smaller insurers an easy way to access a large network of providers.
In 2006, private equity firms began eyeing MultiPlan as a valuable service with few competitors, a market position that only grew after the aforementioned 2010 ACA devlopments. Over the ten years from 2006 to 2016, MultiPlan changed hands between PE firms no fewer than four times. Meanwhile, MultiPlan was also making large acquisitions of competitors and firms in adjacent spaces:
- 2006: MultiPlan acquired by Carlyle Group for $1 billion
- 2006: MultiPlan acquires PHCS, the largest primary care network in the US
- 2010: MultiPlan acquired by BC Partners and Silver Lake for $3.1 billion
- 2010: MultiPlan acquires Viant, another competitor
- 2011: MultiPlan acquires NCN, a reimbursement management platform
- 2014: MultiPlan acquired by Starr Investment Holdings and Partners Group for $4.4 billion
- 2014: MultiPlan acquires Medical Alert & Review, which identifies wasteful billing
- 2016: MultiPlan acquired by Hellman & Friedman for $7.5 billion
Not only did MultiPlan’s value increase by a factor of more than 7 times over 10 years—its owners “cleaned up,” in the words of a Wall Street Journal blog post— it also acquired many of its potential competitors. To my knowledge, MultiPlan no longer has competitors. It’s just MultiPlan and the insurers that use it.
Following some of these acquisitions, MultiPlan expanded its service offerings beyond provider negotiation. The corporation also uses a Palantir-like combination of algorithm and human to root out “fraud and abuse” in payments. And for insurers who worry about what their members think of them, MultiPlan offers a set of analytics services that “balance[s] out-of-network savings and member service.”
From what I can tell, this means MultiPlan has a side business in blocking certain treatments and medications to save the insurer money, or at least making things very hard on doctors who try to prescribe expensive care.
This makes sense from MultiPlan’s perspective, as MultiPlan’s revenue (as far as I can tell—they’re not yet public) comes from a combination of the contract fees that insurers pay to access MultiPlan’s network, in addition to a percentage of the “savings” MultiPlan gets for insurers by routinely lowballing doctors.
Theoretically, MultiPlan’s harsh negotiation tactics should be good for rising American health care costs; insurers are supposed to lower costs by negotiating lower prices on behalf of the patient.
But instead, MultiPlan acts like a mafia enforcer for insurers, forcing doctors to accept low payments while insurance premiums for patients…somehow continue to rise.
MultiPlan’s key strategy for forcing doctors to accept low prices is by erecting a bureaucratic layer so thick and complicated that few can navigate it. On one MultiPlan fax to a doctor that I saw, MultiPlan gave the physician 8 days to respond to a low-ball negotiation. “Please note that if you do not wish to sign the attached proposal,” the fax said, “this claim is subject to a payment as low as 110% of Medicare rate as based on the guidelines and limits on the plan for this patient.”
In other words, if the physician disagrees with MultiPlan’s reimbursement offer, MultiPlan reserves the right to cut the price even lower.
MultiPlan preys on physicians using these subtly forceful faxes, expecting physicians’ medical billing staff to not have time to fight through layers of bureaucratic tape. And according to a friend who works in medical billing, even if a staff member takes it upon themselves to complain about a low rate to MultiPlan, MultiPlan refuses to negotiate on the grounds that it is not the insurer.
Now MultiPlan is going public via a SPAC. There’s a lot of money to be made in leveraging the fragmentation of the health care system and bending physicians to your will, and Churchill Capital looks ready to sweep it up.
Olivia Webb. (2020, August 5). MultiPlan, the secret back-end to most of the insurer industry, is going public. Acute Condition. https://www.acutecondition.com/p/multiplan-the-secret-back-end-to?fbclid=IwAR342wrhyNVpIY_mKp7HY8-6TlwXDFudVrJALD49ZZVvRbBJxdJnTAVyIp8
You may like
-


Health Insurance Use Wordplay to Deceive Providers and Patients
-


Insurance Companies are Being Sued by a Surgery Center that Had Enough
-

“TAKE IT OR LEAVE IT,” IS HURTING PATIENT CARE
-


Hãng bảo hiểm sức khỏe có trả tiền cho giải phẫu thẩm mỹ không?
-


Insurance Companies Working the System
-


“Karma is a Bitch,” But They Had it Coming
Business
AB5 VÀ TÁC ĐỘNG ĐẾN THỢ MÓNG TAY NGƯỜI VIỆT TRONG 2025
Published
2 weeks agoon
July 10, 2024By
admin
AB5 AND ITS IMPACT ON VIETNAMESE MANICURISTS IN 2025
Năm 2019, California đã thông qua Dự luật Quốc hội 5 (AB5), một đạo luật mang tính đột phá nhằm phân loại lại các nhà thầu độc lập là nhân viên trong một số ngành nhất định. Luật này có ý nghĩa sâu rộng trong nhiều lĩnh vực khác nhau, nhưng có lẽ rõ ràng hơn trong ngành làm móng, nơi nhiều thợ làm móng Việt Nam hoạt động với tư cách là nhà thầu độc lập.
AB5 được thiết kế chủ yếu để giải quyết những lo ngại về việc phân loại sai người lao động và để đảm bảo rằng các nhà thầu độc lập nhận được các quyền lợi và sự bảo vệ cho nhân viên. Nó mã hóa “bài kiểm tra ABC”, xác định xem một công nhân có được phân loại đúng là nhà thầu độc lập hay không dựa trên:
1. A – Người lao động có thoát khỏi sự kiểm soát và chỉ đạo của cơ quan tuyển dụng trong việc thực hiện công việc hay không.
2. B – Công việc được thực hiện có nằm ngoài quy trình kinh doanh thông thường của đơn vị tuyển dụng hay không.
3. C – Liệu người lao động có thường xuyên tham gia vào một hoạt động thương mại, nghề nghiệp hoặc kinh doanh được thành lập độc lập hay không.
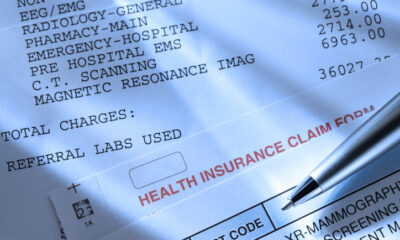
Với sự giúp đỡ của cựu Thượng nghị sĩ Janet Nguyễn, Dự luật Quốc hội 1561 đã tạm thời đình chỉ AB5 trong vài năm để giúp các doanh nghiệp thẩm mỹ viện dễ dàng chấp nhận luật mới nhưng kể từ ngày 1 tháng 1 năm 2025, thợ làm móng sẽ không còn được miễn trừ nữa. Chính trị gia Việt Nam hiện tại duy nhất có thể giúp cộng đồng đề xuất Dự luật mới là Nghị sĩ Trí Tạ, tuy nhiên ông vẫn chưa lên tiếng giúp đỡ các thợ nail sau một năm nhậm chức. Thợ làm móng người Việt chiếm gần 70% lực lượng lao động trong các tiệm nail nên khi luật AB5 có hiệu lực vào năm 2025, Dân biểu Trí Tạ sẽ mất đi phần lớn người Việt ủng hộ ông. Để ngăn luật này có hiệu lực, chúng ta cần anh ấy đứng ra và thực hiện vai trò của mình với tư cách là một chính trị gia được bầu chọn. Nếu không, công dân Mỹ gốc Việt sẽ không bỏ phiếu cho anh ấy và sẽ bỏ phiếu cho một người khác sẵn sàng giúp đỡ các thợ làm móng người Việt trong nhiệm kỳ tới.
Nếu không có luật ngăn chặn AB5, việc phân loại lại có thể đồng nghĩa với những thay đổi đáng kể trong cách các thợ làm móng Việt Nam hoạt động theo cơ chế hoa hồng và sự bảo vệ hợp pháp của họ. Một trong những nhược điểm chính của việc được phân loại là nhân viên theo AB5 là có thể mất đi sự hỗ trợ của chính phủ như phúc lợi, phiếu thực phẩm, trợ cấp mua sắm, nhà ở, hỗ trợ tài chính cho giáo dục hoặc Medi-Cal nếu thu nhập được báo cáo của thợ làm móng cao hơn thu nhập. ngưỡng được phép nhận trợ cấp khi họ sẽ báo cáo mức lương theo giờ. Hầu hết các thợ làm móng kiếm được mức lương W2 sẽ chỉ báo cáo mức lương tối thiểu và phần thu nhập còn lại của họ sẽ được bỏ dưới dạng tiền mặt. Tất nhiên, Bộ Lao động đã được cảnh báo về điều này và sẽ kiểm tra bảng lương của người sử dụng lao động đối với những khoản lương tiềm ẩn chưa được trả, thời gian làm thêm giờ không được trả, thời gian nghỉ ốm không được trả lương, v.v.
Vì vậy, với tư cách là chủ tiệm, những thay đổi đáng kể này có thể dẫn đến tăng chi phí do thuế trả lương, phúc lợi, nguồn nhân lực và khả năng tái cơ cấu mô hình kinh doanh của họ. Bây giờ họ sẽ được kiểm toán và chịu trách nhiệm trước Bộ Lao động. Các tiệm nhỏ hơn có thể gặp khó khăn trong việc giải quyết những khoản chi phí bổ sung này, có khả năng dẫn đến những thay đổi trong cách họ hoạt động hoặc thậm chí đóng cửa.
Động lực trong các tiệm nail cũng có thể thay đổi. Với các thợ làm móng hiện được coi là nhân viên, họ sẽ phải tuân theo lịch trình có cấu trúc chặt chẽ hơn, phải tuân thủ các điều kiện làm việc hạn chế, tuân thủ các quy tắc và hướng dẫn của người sử dụng lao động, và đặc biệt là những thợ làm móng coi trọng tính linh hoạt của việc trở thành nhà thầu độc lập, có thể thấy những thay đổi này bị hạn chế.
Khi chúng ta bước đến năm 2025, tác động đầy đủ của AB5 đối với các thợ làm móng tay Việt Nam sẽ trở nên rõ ràng hơn. Những thách thức như điều chỉnh theo cơ cấu việc làm mới và khả năng phản đối từ các chủ tiệm là rất lớn.
Việc triển khai AB5 đặt ra những thách thức và sự không chắc chắn cho các thợ làm móng người Việt ở California và hơn thế nữa. Cuối cùng, chúng ta sẽ chứng kiến nhiều tiệm đóng cửa và một lượng lớn thợ làm móng rời khỏi California. Bối cảnh phát triển của ngành làm móng sẽ đòi hỏi sự thích ứng từ cả nhân viên và chủ tiệm để thích ứng với những thay đổi này.
—————————————–
In 2019, California passed Assembly Bill 5 (AB5), a groundbreaking legislation aimed at reclassifying independent contractors as employees in certain industries. This law has had far-reaching implications across various sectors, but perhaps more visibly in the nail salon industry, where many Vietnamese manicurists operate as independent contractors.
AB5 was primarily designed to address concerns about worker misclassification and to ensure that independent contractors receive employee benefits and protections. It codifies the “ABC test,” which determines if a worker is properly classified as an independent contractor based on:
1. A – Whether the worker is free from the control and direction of the hiring entity in performing the work.
2. B – Whether the work performed is outside the usual course of the hiring entity’s business.
3. C – Whether the worker is customarily engaged in an independently established trade, occupation, or business.
With the help of former Senator Janet Nguyen, Assembly Bill 1561 temporarily suspended AB5 for a few years to help salon businesses ease into the new law but as of January 1, 2025, manicurists will no longer be exempted. The only current Vietnamese politician that can help the community propose a new Bill is Assemblyman Tri Ta, yet he has not raised his voice to help nail technicians after being in office for a year. Vietnamese Manicurists make up of almost 70% of the workforce in nail salons so when the AB5 law goes into effect in 2025, Assemblyman Tri Ta will lose most of his Vietnamese supporters. In order to prevent this law from going into effect, we need him to step up and do his part as an elected politician. Otherwise, Vietnamese American citizens will not be voting for him and will cast their vote for someone else who is more willing to help the Vietnamese Manicurists in the next term.
Without a law to prevent AB5, reclassification could mean significant changes in how Vietnamese manicurists who operate on a commission basis work and their legal protection. One of the key disadvantages of being classified as an employee under AB5 is the possible loss of government assistance such as welfare, food stamps, shopping allowances, housing, financial aid for education, or Medi-Cal if the manicurist’s reported income is higher than the allowed threshold for benefits now that they will be reporting hourly wages. Most manicurists who do earn W2 wages will only report the minimum wage and the remainder of their earnings will be pocketed as cash. Of course, the Department of Labor has been alerted to this and will be auditing employers payroll for potential unpaid wages, unpaid overtime, unpaid sick leave, etc.
So as a salon owner, these significant changes may lead to increased costs due to payroll taxes, benefits, human resources, and potential restructuring of their business models. They will now be audited and be held accountable by the Department of Labor. Smaller salons might struggle to absorb these additional expenses, potentially leading to changes in how they operate or even closures.
Dynamics within nail salons may also shift. With manicurists now considered employees, they will have to follow more structured schedules, be required to adhere to restrictive working conditions, abide by employer rules and guidelines, and especially manicurists who value the flexibility of being independent contractors, may find these changes restrictive.
As we approach 2025, the full impact of AB5 on Vietnamese manicurists will become clearer. Challenges such as adjusting to new employment structures and potential resistance from salon owners loom large.
The implementation of AB5 poses challenges and uncertainties for Vietnamese manicurists in California and beyond. Eventually, we will see many salon closures and a major exodus of Manicurists moving out of California. The evolving landscape of the nail salon industry will require adaptation from both workers and salon owners alike to navigate these changes.
Business
WHY ARE BIG BANKS LIKE BANK OF AMERICA STUCK UP?
Published
2 months agoon
May 29, 2024By
admin
In the complex world of finance, few institutions stand as pillars of power and authority quite like banks. With their towering buildings, polished marble floors, and tellers behind imposing counters, banks often exude an air of exclusivity and superiority. Why are big banks so stuck up? What lies beneath the veneer of opulence and arrogance?
The culture within banking circles often perpetuates an attitude of elitism and snobbery. High-powered executives in custom-made suits, lavish corporate events, and exclusive networking opportunities create a limited environment where the lines between privilege and arrogance blur. This culture of exclusivity further reinforces the perception of banks as stuck-up institutions.
Banks wield immense financial power, capable of shaping economies and influencing global markets. With this power comes a sense of superiority, as bankers see themselves as the gatekeepers of wealth and prosperity. The ability to approve or deny loans, dictate interest rates, and control the flow of capital instills banks with a sense of invincibility and arrogance.
In an incident on Friday, May 03, 2024, between a regular customer and Bank of America located on Brookhurst and Slater in Fountain Valley, CA when the customer came in to open an account with an $85,0000 check to deposit. Without an explanation as to why he wasn’t able to open an account, two Vietnamese bank employees asked security to escort the customer out of the branch. The employees didn’t bother to explain to him why he was being escorted out nor did they take the time to review his accounts or ask him any questions. It wasn’t like he was withdrawing money, but depositing a check. This customer, who has had several business checking accounts with Bank of America for many years was treated disrespectfully and felt insulted by their actions. Although he was able to take the check to another bank, this incident illustrates how stuck-up banks have become and the lack of customer care. This Bank of America branch acted like they didn’t need the money or the customers.
Bank of America is notorious for its arrogance and for charging high fees. They nickel and dime customers, charge high interest rates on their loans, charge high monthly fees unless a minimum amount of money is in the account, and limited in-branch services. What happened to the days when banks were fighting for customers and offering free accounts? Maybe banks have made too much in the current economy through mortgage loans, credit card debt, the growing stock market, and high interest, they could care less about a few thousand dollars.
Chase Bank in Westminster, CA on Beach and Westminster won’t even open a check account for you if you walk in. You must make an appointment and be able to finish the transaction in the amount of time allotted or you’ll be rescheduled to come back another time. Actions like these banks exacerbate perceptions of arrogance.
Long wait times, impersonal service, and complex bureaucratic procedures create an environment where customers feel marginalized and insignificant. This perceived lack of empathy and understanding reinforces the notion that banks are more concerned with their own interests than those of their customers.
While regulations exist to ensure the stability and integrity of the financial system, they can also contribute to the perception of banks as stuck-up entities. Complex regulatory frameworks create barriers to entry, consolidating power within a select group of institutions. This lack of competition fosters complacency and reinforces the notion that banks are untouchable entities beyond reproach.
The perception of banks as stuck-up institutions is widespread because the actions of a few high-profile banks like Bank of America perpetuate the perception of arrogance within the industry. It underscores the need for banks to prioritize transparency, accountability, and customer-centricity to rebuild trust and reshape their image in the eyes of the public. Only by addressing these underlying issues can banks shed the cloak of arrogance and truly serve the needs of their customers and communities.
TẠI SAO NGÂN HÀNG LỚN NHƯ NGÂN HÀNG BANK OF AMERICA KIÊU NGẠO
Trong thế giới tài chính phức tạp, hiếm có tổ chức nào có thể đứng vững như những trụ cột quyền lực và quyền lực như các ngân hàng. Với những tòa nhà cao chót vót, sàn đá cẩm thạch bóng loáng và những nhân viên thu ngân đằng sau quầy tính tiền uy nghi, các ngân hàng thường toát ra vẻ độc quyền và ưu việt. Tại sao các ngân hàng lớn lại kiêu ngạo như vậy? Điều gì nằm bên dưới vẻ ngoài sang trọng và kiêu ngạo?
Văn hóa trong giới ngân hàng thường duy trì thái độ thượng lưu và hợm hĩnh. Các giám đốc điều hành có quyền lực cao trong những bộ vest được thiết kế riêng, các sự kiện xa hoa của công ty và các cơ hội kết nối độc quyền tạo ra một môi trường hạn chế, nơi ranh giới giữa đặc quyền và sự kiêu ngạo bị xóa nhòa. Văn hóa độc quyền này càng củng cố thêm nhận thức về các ngân hàng như những tổ chức kiêu ngạo.
Các ngân hàng nắm giữ sức mạnh tài chính to lớn, có khả năng định hình nền kinh tế và ảnh hưởng đến thị trường toàn cầu. Quyền lực này mang lại cảm giác vượt trội, khi các chủ ngân hàng coi mình là người gác cổng của sự giàu có và thịnh vượng. Khả năng phê duyệt hoặc từ chối các khoản vay, ấn định lãi suất và kiểm soát dòng vốn khiến các ngân hàng có cảm giác bất khả chiến bại và kiêu ngạo.
Trong một sự cố xảy ra vào Thứ Sáu, ngày 03 tháng 5 năm 2024 giữa một khách hàng thường xuyên và Bank of America ở Brookhurst và Slater ở Fountain Valley, CA khi khách hàng đến mở tài khoản với khoản tiền gửi check là 85.000 USD. Không giải thích lý do không mở được tài khoản, hai nhân viên ngân hang người Việt đã yêu cầu bảo vệ hộ tống khách hàng ra khỏi chi nhánh. Các nhân viên chi nhánh không thèm giải thích cho anh ta lý do tại sao anh ta bị áp giải ra ngoài cũng như không dành thời gian để xem xét tài khoản của anh ta hay hỏi anh ta bất kỳ câu hỏi nào. Anh ta không cố gắng rút tiền mà muốn gửi check. Khách hàng này có nhiều tài khoản check kinh doanh với Bank of America trong nhiều năm, đã bị đối xử thiếu tôn trọng và cảm thấy bị xúc phạm bởi hành động của họ. Mặc dù anh ấy đã mang tấm check này đến một ngân hàng khác và mở một tài khoản kinh doanh mới ngay sau đó, nhưng sự việc này cho thấy các ngân hàng kiêu ngạo như thế nào và thiếu sự chăm sóc khách hàng. Chi nhánh Bank of America này hành động như thể không cần tiền hay khách hàng.
Bank of America nổi tiếng vì sự kiêu ngạo và tính phí cao. Họ tính phí cho khách hàng, tính lãi suất cao cho các khoản vay của họ, tính phí hàng tháng cao trừ khi có số tiền tối thiểu trong tài khoản và hạn chế các dịch vụ tại chi nhánh. Điều gì đã xảy ra vào thời mà các ngân hàng đấu tranh vì khách hàng và cung cấp tài khoản miễn phí? Có thể các ngân hàng đã kiếm được quá nhiều trong nền kinh tế hiện tại thông qua các khoản vay thế chấp, nợ thẻ tín dụng, thị trường chứng khoán đang phát triển và lãi suất cao, họ có thể không quan tâm đến vài nghìn đô la.
Ngân hàng Chase ở Westminster, CA trên Beach và Westminster thậm chí sẽ không mở tài khoản séc cho bạn nếu bạn bước vào. Bạn phải đặt lịch hẹn và có thể hoàn tất giao dịch trong khoảng thời gian quy định nếu không bạn sẽ bị dời lịch đến hãy quay lại vào lúc khác. Những hành động như thế này của các ngân hàng làm trầm trọng thêm nhận thức về sự kiêu ngạo.
Thời gian chờ đợi lâu, dịch vụ không mang tính cá nhân và các thủ tục quan liêu phức tạp tạo ra một môi trường nơi khách hàng cảm thấy bị thiệt thòi và tầm thường. Sự thiếu đồng cảm và hiểu biết này càng củng cố quan điểm cho rằng các ngân hàng quan tâm đến lợi ích của chính họ hơn là lợi ích của khách hàng.
Mặc dù các quy định tồn tại để đảm bảo sự ổn định và toàn vẹn của hệ thống tài chính, nhưng chúng cũng có thể góp phần tạo ra nhận thức về các ngân hàng như những thực thể đang mắc kẹt. Các khung pháp lý phức tạp tạo ra các rào cản gia nhập, củng cố quyền lực trong một nhóm các tổ chức được lựa chọn. Sự thiếu cạnh tranh này thúc đẩy sự tự mãn và củng cố quan điểm cho rằng các ngân hàng là những thực thể không thể chạm tới, không thể chê trách được.
Quan niệm coi các ngân hàng như những tổ chức bế tắc đang lan rộng, bởi vì hành động của một số ngân hàng nổi tiếng như Bank of America đã kéo dài thêm nhận thức về sự kiêu ngạo trong ngành. Nó nhấn mạnh sự cần thiết của các ngân hàng phải ưu tiên tính minh bạch, trách nhiệm giải trình và lấy khách hàng làm trung tâm để xây dựng lại niềm tin và định hình lại hình ảnh của họ trong mắt công chúng. Chỉ bằng cách giải quyết những vấn đề cơ bản này, các ngân hàng mới có thể rũ bỏ tấm áo kiêu ngạo và thực sự phục vụ nhu cầu của khách hàng và cộng đồng của họ.
Business
FBI INVESTIGATORS ARE CREATING CRIMINALS
Published
11 months agoon
August 21, 2023By
admin
Dr. Robert Joseph, a podiatrist in California, who was indicted by the United States District Court for the Central District of California for the illegal practice of colluding with pharmaceutical marketers for writing prescriptions of compounding drugs, is now working undercover for the FBI. In exchange for a lower sentence due to his indictment in 2018, Dr. Robert Joseph is now working undercover to deceive medical facilities and doctors by intentionally offering illegal deals.
This article is to help warn medical facilities and doctors of the devious practice that the FBI is taking to catch them in the act. It is one thing to investigate incidences due to patient complaints or whistleblowers but to intentionally embed a mole to create a problem when there is no problem, this is how the FBI works. If Adam is tempted by the apple because it was offered is that the same as if he had already bit the apple without the temptation created by Eve? In this case, the FBI is going fishing in hopes of finding something.
A medical facility in Huntington Beach, CA was a victim of Dr. Robert Joseph and the FBI. Dr. Joseph came into the facility wearing a concealed camera and had the intention of catching them by offering an illegal deal. Fortunately, this medical facility did not take the bait but wanted to share their experience with the public so that other medical offices and doctors will be aware of Dr. Robert Joseph.
As the public, we want doctors to care about us and to do what’s best for us and not be greedy. That is the oath they take when they become doctors. There are doctors who are tempted to sway but being tempted versus actually acting on greed is not the same. What the FBI is doing is turning the tempted into greedy criminals.
Ref: https://www.justice.gov/file/1076086/download

AB5 VÀ TÁC ĐỘNG ĐẾN THỢ MÓNG TAY NGƯỜI VIỆT TRONG 2025

TÔI GAY KHÔNG CÓ NGHĨA LÀ TÔI HẤP DẪN VỚI TẤT CẢ ĐÀN ÔNG

KIỂM SOÁT VÀ SỰ XÓI MÒN QUYỀN TỰ DO BIỂU TƯỢNG Ở VIỆT NAM
Trending
-
 Politics3 years ago
Politics3 years agoAssemblywoman Janet Nguyen Announces Election Bid in Newly Drawn Senate District
-

 Business2 years ago
Business2 years agoCalifornia Gov. Newsom says community spread started at nail salon
-

 Business3 years ago
Business3 years agoInsurance Companies Working the System
-

 Business3 years ago
Business3 years agoUCLA: Ngành nail Việt Nam ở California bị đại dịch COVID-19 ảnh hưởng nặng
-

 Business3 years ago
Business3 years agoLee’s Sandwiches recalls meat after federal inspection
-

 Business4 years ago
Business4 years agoBác sĩ thẩm mỹ xài chứng chỉ hành nghề giả, làm chết bệnh nhân ở Sài Gòn
-

 Business3 years ago
Business3 years agoTiệm nail Việt ở California đòi chính quyền bồi thường thiệt hại $5 triệu
-

 Health3 years ago
Health3 years agoHãng bảo hiểm sức khỏe có trả tiền cho giải phẫu thẩm mỹ không?